Clinical Brain Injury Research at Pate Rehabilitation
Through our brain injury research, we contribute to the body of knowledge surrounding brain injury rehabilitation. Pate professionals collaborate in research projects with nationally recognized institutions, contribute to top tier research publications and present their findings at national conferences.
Current Studies, Publications, and Presentations
2020
Perea, J. D., & Salisbury, D. (2020). Seamless integration of client-centered technology into the neuro-rehabilitation setting. American Congress of Rehabilitation Medicine Annual Conference, Virtual Oct. 19-24.
Tucker, J,. S., & Salisbury, D. (2020). From rehabilitation laboratory to real world independence.
American Congress of Rehabilitation Medicine Annual Conference, Virtual Oct. 19-24.
Burns, S, Perea, J. D., Terblanche, M., Lillard, H. M., De La Pena, C., & Grinage, N. (2020). mHealth Apps: Examining the Difference between Availability and the Evidence. Presented at the American Congress of Rehabilitation Medicine Annual Conference, Virtual, Oct. 19-24
Carolyn Cassill, B.S., Carlos Marquez de la Plata, Ph.D., and Mary Anise Psy.D.(2020). Balancing Patient Autonomy and Medical Paternalism in Rehabilitation Treatment Planning . Presented at the American Congress of Rehabilitation Medicine Annual Conference, Virtual, Oct. 19-24
Hreha, K., Rizzo, J.R., Roberts, P., Wertheimer, J, Perea, J., Weden, K., Watters, K., & Llanos, I. (2020). Feasibility and Validity of a Vision Screening Tool: A Multi-Site Study. Presented at the American Congress of Rehabilitation Medicine Annual Conference, Virtual, Oct. 19-24
Kringle, E., Illva, H., Hay, C., Perea, J., Baratta, J., & Frias, A. (2020). From Disability to Productivity: Transitioning to Employment, Volunteerism, and Caregiving following Stroke. Presented at the American Congress of Rehabilitation Medicine Annual Conference, Virtual, Oct. 19-24
Meredith, K. & Perna, R. (2020). Dignity of risk following brain injury. Brain Injury Association of America, Live Webinar 9/24/2020
Salinas, P, Goff, A., and Featherston, J. (2020). Interdisciplinary Rehab: An Approach to Return to Work. Presented at the American Congress of Rehabilitation Medicine Annual Conference, Virtual, Oct. 19-24.
2019
Featherston, J. (2019). Vocational Rehabilitation for Acquired Brain Injuries. Presented at Brain Injury Association of Louisiana Conference. New Orleans, LA, Mar. 29-30.
Featherston, J. (2019). Navigating the RTW process for clients with ABI. Presented at the Case Management Society of America National Conference. Las Vegas, NV, June 10-14.
American Congress of Rehabilitation Medicine (ACRM) Annual Conference, 2019
POSTER
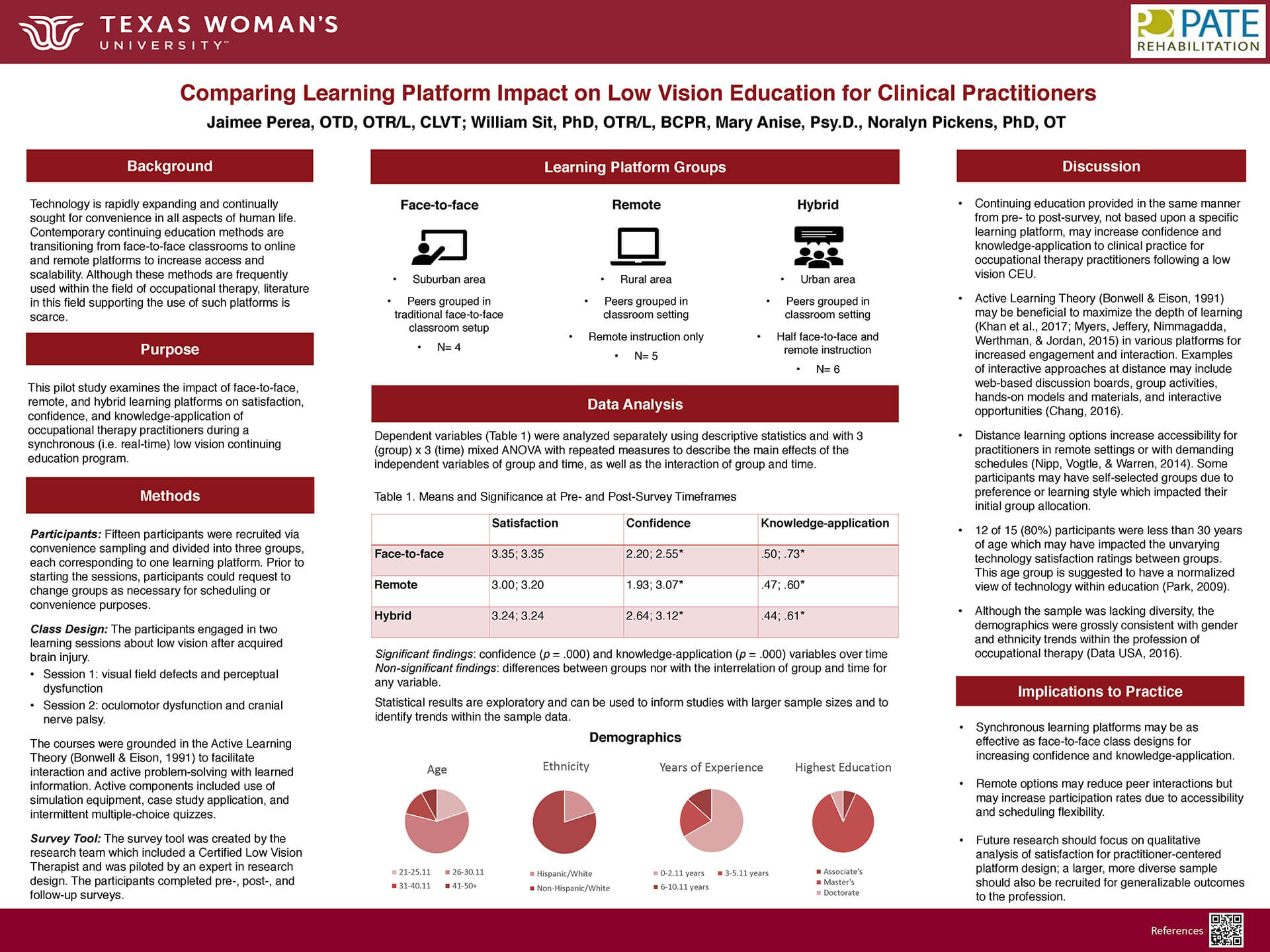
Comparing the Impact of Learning Platform on Low Vision Continuing Education for Clinical Practitioners
Primary Author: Jaimee Perea, OTR, OTD, CLVT, CBIS
Coauthors: Mary Anise, Psy.D.
Purpose: To outline the impact of face-to-face, online, and hybrid learning platforms on satisfaction, confidence, and knowledge-application of clinical practitioners during a synchronous low vision continuing education program.
Summary: This pilot study used a three-group repeated measure design to compare the impacts of group and time on the dependent variables. A private clinic and public hospital were used for the sessions in urban, suburban, and rural settings dependent upon the group. Participants (n=15) were current occupational therapy (OT) practitioners recruited using convenience sampling and grouped based on their location and scheduling. 53 participants were screened for eligibility based upon inclusion criteria of English language fluency, current practitioner in Dallas/Fort Worth, TX, access to a wifi capable device, and aged 21 years of or older. Participants engaged in two synchronous 45-minute education sessions about low vision after acquired brain injury. Pre-, post-, and follow-up survey were administered at designated time-points. A survey was developed to assess satisfaction with technology used, confidence with acquired knowledge translation to practice, and knowledge-application to clinical scenarios with a four-point Likert Scale. Significance was found between pre- and post-survey timepoints of the study for confidence (p<.001) and knowledge-application (p<.001) variables. No significance was found between face-to-face, online, and hybrid groups. Data demonstrated 88% retention rate to inform a future scaled study. This pilot study showed that there may be no difference between learning platforms with synchronous and consistently presented information during continuing education courses. Despite learning platform used, learners may still increase their knowledge and confidence translating acquired information to practice. Distance options provide greater flexibility to allow greater participation and convenience with learning.
POSTER
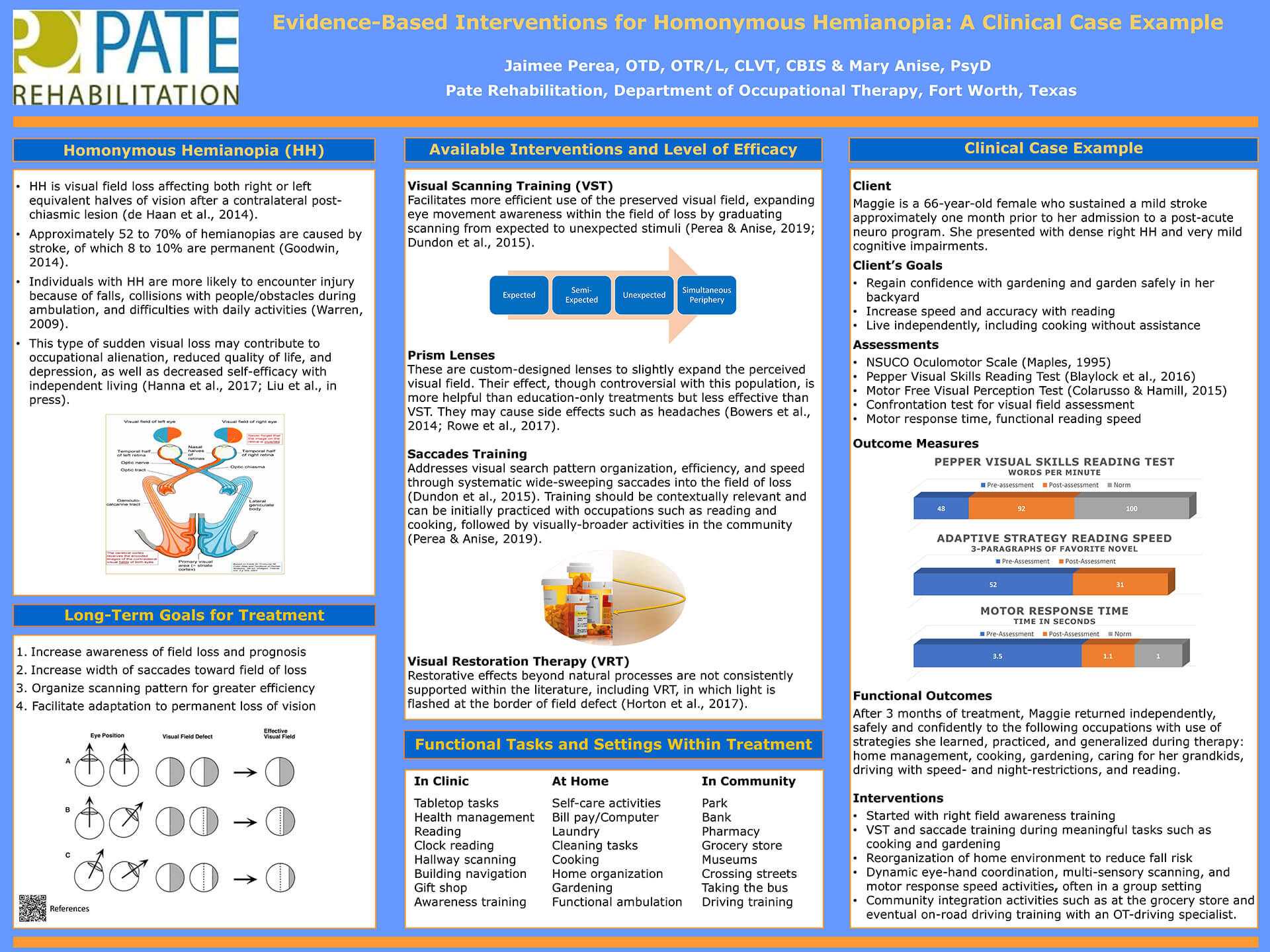
Evidence-Based Interventions for Homonymous Hemianopia (HH): A Clinical Case Example
Primary Author: Jaimee Perea, OTR, OTD, CLVT, CBIS
Coauthors: Mary Anise, Psy.D.
Purpose: To improve the knowledge base of OT practitioners by: 1) reviewing evidence-based interventions for adults with HH and 2) illustrating implementation of such approaches through a successful case example.
Summary: This involved an intervention case study with before and after assessments completed within a three-month period of treatment. The study occurred within a private post-acute brain-injury rehabilitation setting. The subject of the study was a 66-year-old Caucasian female who sustained a stroke one month prior to her admission on referral from a physician. Interventions included Visual Scanning Training (VST) that involved the following: right field awareness training, re-organizing environments to reduce fall risk and increase success with task completion, eye-hand coordination and dynamic scanning in a group setting to increase comfort with social participation, application of skills inside buildings and within the community, practice with adaptive equipment and strategies, and integration of multi-sensory experiences to support resumption of occupations with complex environmental demands. Outcome Measures included: Pepper Visual Skills Reading Test, visuomotor response time, behind-the-wheel driving evaluation, and assessment of return to meaningful occupations. After these interventions were implemented, the patient’s Pepper-VSRT improved from 48 to 92 words per minute. Resumption of reading was possible with 90-degree book tilting. 3-paragraph pace improved from 52 to 31 seconds. Visuomotor response time improved from 3.5 to 1.1 seconds. Subject was cleared to drive with some restrictions after hours of behind-the-wheel interventions with an OT specializing in driver rehabilitation. The patient successfully resumed living independently, cooking, and gardening. This case study illustrates that OTs are uniquely equipped to teach individuals VST as a response to a positive assessment for HH. Individuals report greater confidence with occupations in their homes and communities as a result of evidence- and activity-based OT intervention.
 Culturally Competent Rehabilitation
Culturally Competent Rehabilitation
Dr. Carlos Marquez de la Plata gave a continuing education talk at the Louisiana chapter of the Brain Association of America in March, 2018.
The hour long talk, called "What is Culturally Competent Rehabilitation?" addressed disparities in rehabilitation outcomes with a discussion of implicit biases. Dr. Marquez de la Plata described ways clinicians can become more aware of various cultural preferences and values and how to adapt their therapy skills to match the patients’ values. The talk also covered several ways to modify therapies to take more of a a client-centered approach and improve the way clinicians demonstrate respect for patients’ autonomy, a collaborative approach, and desire to empower patients.
American Psychological Association Division 22 Annual Meeting, 2018
POSTER
 Return to Work Outcomes After Post-Acute Rehab Following Stroke and Traumatic Brain Injury
Return to Work Outcomes After Post-Acute Rehab Following Stroke and Traumatic Brain Injury
Primary Author: Gail Darden
Coauthors: Paige Salinas, Jessica Woods, Jeanine M. Galusha, Carlos Marquez de la Plata
Purpose: To evaluate the rate of return to work following comprehensive interdisciplinary post-acute rehabilitation programming for patients with stroke (CVA) and traumatic brain injury (TBI).
Summary: Our clinician-researchers examined 64 consecutive patients admitted to Pate Rehabilitation from February to December 1, 2017 and received a three-stage approach to interdisciplinary therapy that includes (1) assessment, (2) neurofunctional intervention, and (3) work training to optimize employment re-entry. This structured and tiered approach significantly contributes to successful return to work outcomes after an acquired brain injury, as . only 5% of individuals with CVA were working at the time of admission to rehabilitation, and this rate increased to 46% by discharge. Likewise, only 4% of individuals with TBI were working at admission to rehabilitation, and this rate increased to 20% by discharge. These rates are at least commensurate if not better than the rates of return to work reported in this literature.
POSTER
 Driving Outcomes Following Post-acute Stroke Rehabilitation
Driving Outcomes Following Post-acute Stroke Rehabilitation
Primary Author: C. Lighthill
Coauthors: C. Nelson, J. Woods, P. Salinas, C. Marquez de la Plata
Purpose: To examine the effectiveness of Pate’s comprehensive interdisciplinary brain injury rehabilitation programming aimed toward assisting patients’ return to driving goals.
Summary: Our clinician-researchers examined 64 consecutive patients admitted to Pate Rehabilitation from February to December 1, 2017 and received formalized return to driving programming. The return to driving program utilizes a series of evaluations, education, cognitive remediation, and behind the wheel training that is tailored to the individual’s strengths and challenges. Using this hybrid approach of in-clinic and on-the-road experiences, our patients achieve their stated driving goal at an amazing rate. For example, approximately 2.6% of patients with strokes are driving at admission; however, upon discharge, approximately 62% of patients with a driving goal pass the behind the wheel evaluation conducted while in rehabilitation.
POSTER
 Biofeedback Cotreatment Addressing Foot Drop of Stroke Survivors
Biofeedback Cotreatment Addressing Foot Drop of Stroke Survivors
Primary Author: J. Downum
Coauthors: J. Yeager, A. Johnson, K. McWilliams, C. Marquez de la Plata
Purpose: Due to stroke, daily functioning can be compromised. Ambulation and balance are often impaired. Biofeedback is an integrative therapy applied during rehabilitation of musculature. With neuroplasticity and rehabilitation, devices may be eliminated.
Surface Electromyography (SEMG) Biofeedback is an adjunctive therapy providing information about weak muscles through visual and audio feedback. Biofeedback therapist and physical therapist often cotreat during the neurorehabilitation utilizing visual and audio feedback about musculature to build body awareness. Neuroplasticity occurs and when appropriately applied, neuromuscular rehabilitation can improve patient independence (Bolek, 2010). This study evaluated the combination of physical therapy and biofeedback as an intervention for foot drop with stroke survivors.
Summary: Our biofeedback specialist teamed up with several of our physical therapists to co-treat four patients with foot drop, a condition of weakness or paralysis of the muscles involved in lifting the front part of the foot.
The intervention was designed to help the patient build a sense of awareness of how much and how well they are moving their impaired foot during physical therapy to reinforce the efforts involved in walking correctly. This treatment utilizes sensors placed on the patient’s leg that detects neuromuscular activity and projects the amount of activity onto a computer screen to alert the patient when they have sufficiently activated the muscle.
As this is a pilot study of a novel intervention, preliminary results demonstrate auditory and visual feedback can be used to improve range of motion at the foot and walking distance when used as an adjunct to traditional physical therapy for foot drop after stroke. Just as important, patients also reported increased awareness and reduction in foot drag with this therapy. Additionally, they viewed biofeedback cotreatment with PT as helpful. Further examination of this promising therapy with an increased sample size and more rigorous design is recommended.
POSTER
 Effectiveness of Post Acute Interdisciplinary Rehabilitation in Those with Acquired Brain Injury
Effectiveness of Post Acute Interdisciplinary Rehabilitation in Those with Acquired Brain Injury
Jeff Schaffert(1), Jeanine Galusha(2), Carlos Marquez de la Plata(1,2)
UT Southwestern Medical Center Department of Psychiatry(1), Pate Rehabilitation Center(2)
Summary: Patients with traumatic brain injury (TBI) and cerebrovascular accidents (CVA) can suffer chronic physical and cognitive deficits. Intensive post-hospital (post-acute) rehabilitation efforts have been shown to improve functional abilities following these injuries (Turner-Stokes et al., 2015) Various models of post-acute rehabilitation are used, with one relatively uncommon model being “milieu-oriented.” Within these settings, very little is known regarding patient's functional outcomes or the model’s overall effectiveness. Thus, the primary aim of this study was to evaluate functional improvements in patients with TBI and CVA admitted to a milieu-oriented comprehensive post-acute rehabilitation program.
Conclusions:
- All of the improvements reached at least a minimally clinically important difference, and the majority of scores were consistent with a robust clinically important
- Results suggest that on average, patients who attended a milieu-oriented program made significant functional improvements in areas related to ability, adjustment to injury, and
- Future studies should examine specific factors related to improvement within a milieu-oriented setting (e.g., injury characteristics, time since injury, age at injury, cultural, )
- Research comparing models of post-acute rehabilitation are needed, and comparisons across different models would further serve to investigate the effectiveness of a milieu-oriented rehabilitation
 Pate Clinical Director Dr. David Salisbury is one of the authors of an abstract on virtual reality and neurorehabilitation that will be presented at the 4th Annual Federal Interagency Conference on Traumatic Brain Injury. The upcoming symposium takes place in the summer of 2018 in Washington, D.C.
Pate Clinical Director Dr. David Salisbury is one of the authors of an abstract on virtual reality and neurorehabilitation that will be presented at the 4th Annual Federal Interagency Conference on Traumatic Brain Injury. The upcoming symposium takes place in the summer of 2018 in Washington, D.C.
Dahdah, M., Bennett, M., Prajapati, P., Parsons, T., Sullivan, E., Driver, S., Salisbury, D. (2018). The Impact of Virtual Reality on Executive Functioning Training and Association With Neurorehabilitation Outcomes.
 Dr. Carlos Marquez de la Plata co-authored an article published in Neuroprotection in Critical Care and Perioperative Medicine (October 2017).
Dr. Carlos Marquez de la Plata co-authored an article published in Neuroprotection in Critical Care and Perioperative Medicine (October 2017).
Imaging Assessment of Brain Injury was written by Matthew A. Warner, Carlos Marquez de la Plata, David S. Liebeskind, and Ramon Diaz-Arrastia.
Biofeedback and Stroke Recovery
Pate biofeedback therapist Jana Downum conducted a study to evaluate the use of biofeedback during physical therapy to address foot drop in stroke patients. The study provided additional biofeedback therapy in stroke survivors’ regular physical therapy regime. The initial data suggests a positive effect with gains observed in several patients, including better control of the foot and ability to walk longer distances. Currently, Jana is co-treating with Physical therapy, Occupation therapy, and Speech therapy helping patients regulate physiology during treatment.
 Jana has an M.A. from Texas Tech University and a Ph.D. from the College of Integrative Medicine and Health Sciences at Saybrook University.
Jana has an M.A. from Texas Tech University and a Ph.D. from the College of Integrative Medicine and Health Sciences at Saybrook University.
Gait Study
Jessica and Jenna Yeager conducted a study on tape gait training in a sample of 11 post-acute stroke patients. Their study confirmed that applying a simple treatment often used in Parkinson's treatment was highly effective.
Results presented at The International Brain Injury Association’s World Congress in 2017. View the poster.
2,501 PERPOS Validation Study Participants
Pate's innovative PERPOS measuring tool was validated by the peer reviewed journal, NeuroRehabilitation. The PERPOS is a tool for defining structure and distractions within a given environment used by rehabilitation therapists to modify treatment environments and to track progress in functioning within various environments.
The study found a strong association between the MPAI-4 total score and the PERPOS total score suggesting the instrument has very good validity for use with brain injured individuals.
Marquez de la Plata, C., Qualls, D., Plenger, P., Malec, J., Hayden, M. (2017). Ecologically Relevant Outcome Measure for Post-Inpatient Rehabilitation. Neurorehabilitation, doi: 10.3233/NRE-161403
Presentation
![]() Paige Salinas, LCSW, CBIS, Jennifer Featherston, Ph.D., LPC, CRC, CVE, (EAGALA Certified), and Carlos Marquez de la Plata, Ph.D. presented Patient-Centered Vocational Rehabilitation for Individuals With Acquired Brain Injuries.
Paige Salinas, LCSW, CBIS, Jennifer Featherston, Ph.D., LPC, CRC, CVE, (EAGALA Certified), and Carlos Marquez de la Plata, Ph.D. presented Patient-Centered Vocational Rehabilitation for Individuals With Acquired Brain Injuries.
American Congress of Rehabilitation Medicine’s 94th Annual Conference in Atlanta, October 2017
Presentation
![]() Dr. Carlos Marquez de la Plata presented a collaborative project with individuals from Brown University, ABI in New Zealand, and NYU: Community Reintegration in Low-Resource Settings: Unmet Needs and Family Participation in Rehabilitation Process.
Dr. Carlos Marquez de la Plata presented a collaborative project with individuals from Brown University, ABI in New Zealand, and NYU: Community Reintegration in Low-Resource Settings: Unmet Needs and Family Participation in Rehabilitation Process.
2017 American Congress of Rehabilitation Medicine 94th Annual Conference
BIAA Position Paper
 Dr. Carlos Marquez de la Plata was one of the authors of a clinical paper for the non-profit Brain Injury Association of America.
Dr. Carlos Marquez de la Plata was one of the authors of a clinical paper for the non-profit Brain Injury Association of America.
Cioe, N., Seale, G., Marquez de la Plata, C., Groff, A., Gutierrez, D., Ashley, M., Connors, S. (2017). Brain Injury Rehabilitation Outcomes: A Position Paper of the Brain Injury Association of America.
Publications
 Perea, J., & Sit, W. (2020). Comparing Learning Platform Impact on Low Vision Education for Occupational Therapists. The Open Journal of Occupational Therapy, (in press).
Perea, J., & Sit, W. (2020). Comparing Learning Platform Impact on Low Vision Education for Occupational Therapists. The Open Journal of Occupational Therapy, (in press).
 Perea, J. D., Anise, M. C., & Burns, S. P. (2018). Community vision interventions for adults with acquired brain injury. OT Practice, 23(20), 20-23.
Perea, J. D., Anise, M. C., & Burns, S. P. (2018). Community vision interventions for adults with acquired brain injury. OT Practice, 23(20), 20-23.
 Pate Rehabilitation's innovative PERPOS tool was validated in the peer reviewed journal, Neurorehabilitation. Marquez de la Plata, C., Qualls, D., Plenger, P., Malec, J., Hayden, M. (2017).
Pate Rehabilitation's innovative PERPOS tool was validated in the peer reviewed journal, Neurorehabilitation. Marquez de la Plata, C., Qualls, D., Plenger, P., Malec, J., Hayden, M. (2017).
Ecologically Relevant Outcome Measure for Post-Inpatient Rehabilitation. Neurorehabilitation, doi: 10.3233/NRE-161403 (2017)
Publications
 Perea, J., & Anise, M. (2019). Beyond cueing to the left and a red line: Treatment methods for homonymous hemianopia. SIS Quarterly Practice Connections, 4(2), 28-30.
Perea, J., & Anise, M. (2019). Beyond cueing to the left and a red line: Treatment methods for homonymous hemianopia. SIS Quarterly Practice Connections, 4(2), 28-30.
 Plenger, P., Krishnan, K., Cloud, M., Bosworth, C., Qualls, D., Marquez de la Plata, C. published fNIRS-based Investigation of the Stroop Task after TBI in Brain Imaging & Behavior, 10, 357-366. (2016)
Plenger, P., Krishnan, K., Cloud, M., Bosworth, C., Qualls, D., Marquez de la Plata, C. published fNIRS-based Investigation of the Stroop Task after TBI in Brain Imaging & Behavior, 10, 357-366. (2016)